Filip Gnesin 1, Anne Cathrine Baun Thuesen 2 3, Lise Katrine Aronsen Kähler 4, Sten Madsbad 5, Bianca Hemmingsen 6
Main idea: There is no clear evidence whether metformin monotherapy compared with no intervention, behaviour changing interventions or other glucose-lowering drugs influences patient-important outcomes.
Abstract
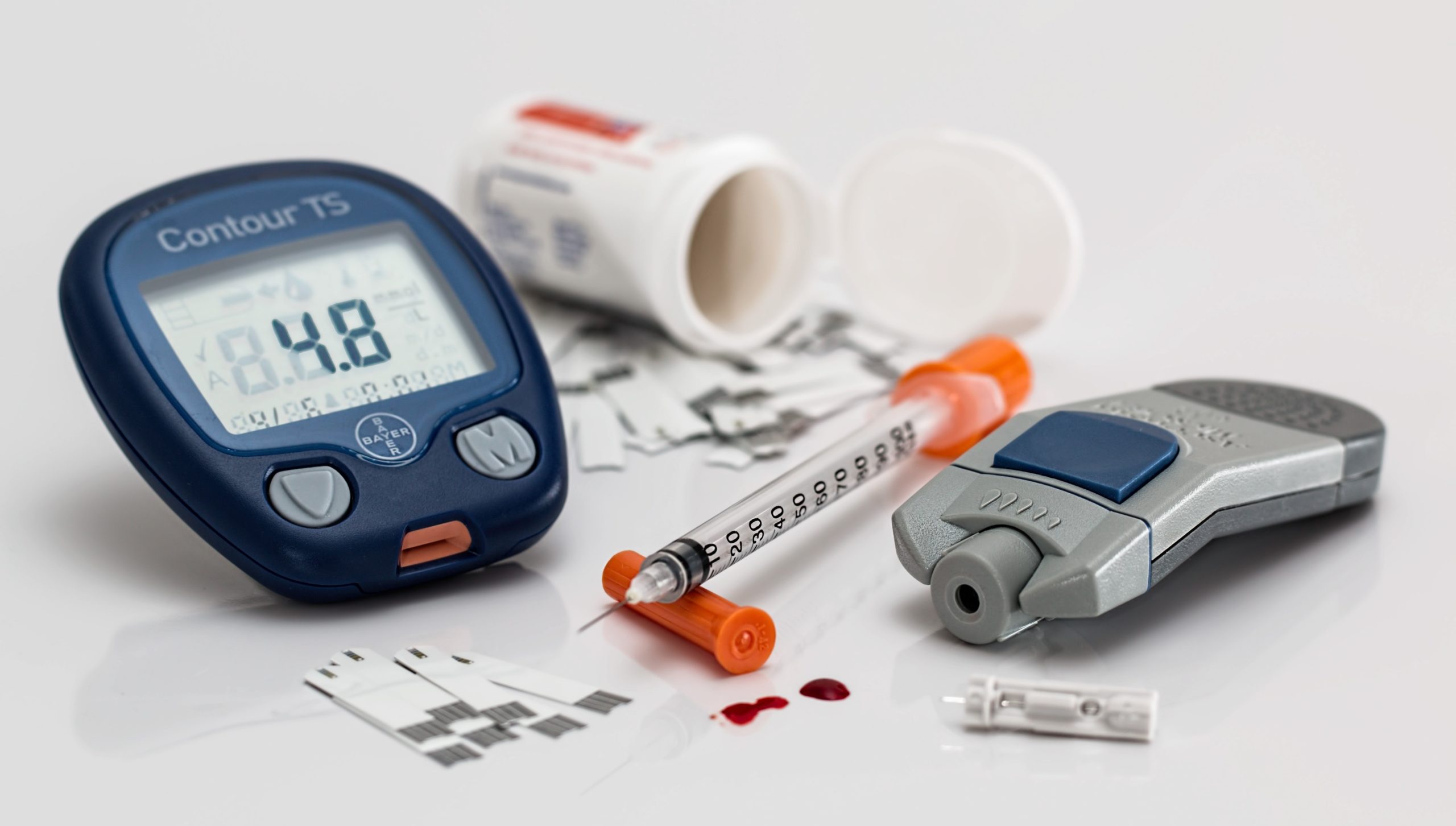
Background: Worldwide, there is an increasing incidence of type 2 diabetes mellitus (T2DM). Metformin is still the recommended first-line glucose-lowering drug for people with T2DM. Despite this, the effects of metformin on patient-important outcomes are still not clarified.
Objectives: To assess the effects of metformin monotherapy in adults with T2DM.
Search methods: We based our search on a systematic report from the Agency for Healthcare Research and Quality, and topped-up the search in CENTRAL, MEDLINE, Embase, WHO ICTRP, and ClinicalTrials.gov. Additionally, we searched the reference lists of included trials and systematic reviews, as well as health technology assessment reports and medical agencies. The date of the last search for all databases was 2 December 2019, except Embase (searched up 28 April 2017).
Selection criteria: We included randomised controlled trials (RCTs) with at least one year’s duration comparing metformin monotherapy with no intervention, behaviour changing interventions or other glucose-lowering drugs in adults with T2DM.
Data collection and analysis: Two review authors read all abstracts and full-text articles/records, assessed risk of bias, and extracted outcome data independently. We resolved discrepancies by involvement of a third review author. For meta-analyses we used a random-effects model with investigation of risk ratios (RRs) for dichotomous outcomes and mean differences (MDs) for continuous outcomes, using 95% confidence intervals (CIs) for effect estimates. We assessed the overall certainty of the evidence by using the GRADE instrument.
Main results: We included 18 RCTs with multiple study arms. Treatment duration ranged from one to 10.7 years. No trials were judged to be at low risk of bias on all ‘Risk of bias’ domains. The main outcomes of interest were all-cause mortality, serious adverse events, health-related quality of life and cardiovascular mortality. Seven trials compared metformin with sulphonylureas. Four trials reported on all- Cause mortality. In three trials no participant died, and in the remaining trial 31/1454 participants (2.1%) in the met formin group died. Three trials reported on SAE: in two trials no SAE occurred. Three trials reported no NFMI; one trial reported no NFS occurred. No trial reported on HRQoL or ESRD. Seven trials compared metformin with thiazolidinediones (very low-certainty evidence for all outcomes) Five trials reported all-cause mortality. There was no substantial difference between the interventions for all-cause mortality, SAE, CVM, NFMI and NFS (very low-certainty evidence for all outcomes) No trial reported on HRQoL or ESRD. In one trial 21/1454 participants in the metformin group experienced a NFMI compared with 25/1456 participants (1.7%) in the thiazolidinedione group. One trial reported no NFS occurred. There was no substantial difference between the interventions for all-cause mortality, CVM, NFMI and NFS. Four ongoing trials with 5824 participants are likely to report one or more of our outcomes of interest. HRQoL or ESRD were not reported. No deaths or SAEs occurred (very low-certainty evidence) No other patient-important outcomes were reported.
Source NIH












Leave a Reply
You must be logged in to post a comment.