Causes
The vascular complications of diabetes, those that affect your blood vessels (diabetic angiopathy), are the most significant manifestations of the disease. For example, atherosclerosis (plaque formation in arteries) is the main reason for impaired life expectancy in patients with diabetes. In addition, diabetic kidney disease and retinopathy (a condition affecting part of the eye called the retina) are major contributors to severe renal disease and blindness, respectively.
Abnormal glucose metabolism, associated with high blood sugar levels, leads to complications that affect large blood vessels (macrovascular) or small vessels (microvascular). Macrovascular diabetic angiopathies are mainly related to cardiovascular and cerebrovascular systems. In contrast, microvascular angiopathies include kidney disorders, retinopathy, and nervous system conditions.
Diabetic feet
Diabetic feet, or diabetic ulcer, is a severe complication of diabetes and leads to the overall worse health condition of patients. For people with type 1 or type 2 diabetes, the total lifetime risk of developing diabetic foot ulcer complications is as high as 25%. However, since the initiating factor is often a minor trauma, a diabetic ulcer may be prevented. In addition, early detection of skin injuries can also improve the situation and decrease the risk of disease progression.
Two main causes of diabetic ulcers are atherosclerosis and diabetic peripheral neuropathy. Atherosclerosis is characterized by decreased blood flow in large and medium-sized vessels, loss of elasticity, thickening of the capillary membranes, and deposition of lipids within the walls. Further, it can lead to restricted blood flow in small vessels. Diabetes-related peripheral nervous system disorder affects the sensory, motor, and autonomic nervous systems. Nerve damage makes it harder to feel pain or other symptoms of ulcers or infections. That can cause complications before any problems are noticed.
Ulcers pose a high risk to health because they may lead to severe infections or even gangrene (death of tissue). In some cases, the only way to treat them is to amputate the affected area. Most often, ulcers affect feet and legs, but they can also form in other areas, such as hands or in walls of the stomach.
Symptoms
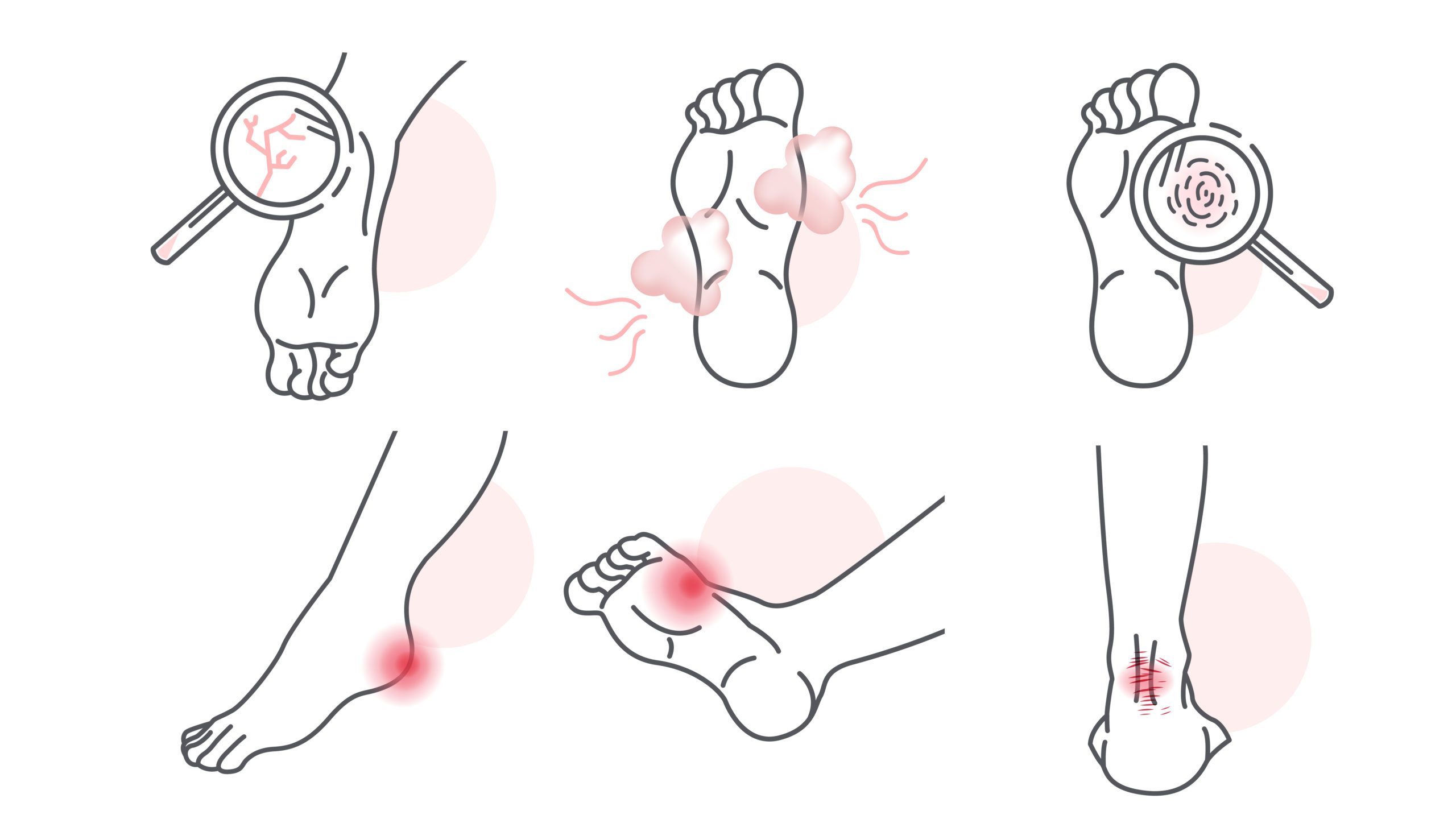
Symptoms may include the following:
- skin color change
- skin temperature change
- the foot or ankle swelling
- leg pain
- corns or calluses
- open wounds that are slow to heal or are draining
- ingrown toenails or toenails with fungus infection
- dry cracks in the skin, particularly around the heel
- unusual or persistent foot odor
Prevention
Profilactics of any complications is essential for patients with diabetes. To prevent foot ulcers, you should:
- daily inspect both feet, including the area between the toes, or ask a caregiver to do it if you are not able to do so;
- wash your feet daily with water at room temperature, carefully dry after washing, especially between the toes;
- cut nails straight across;
- use moisturizers for dry skin, but not between the toes;
- do not remove corns and calluses; they should be treated by trained staff;
- avoid walking barefoot;
- always wear socks with shoes and ensure there are no foreign objects inside before wearing them;
- have regular feet examinations performed by a qualified healthcare provider;
- notify the healthcare provider if a cut, scratch, blister, or sore develops.
Disease management
When dealing with diabetes complications such as ulcers, various aspects should be taken into consideration.
Patient education: information about foot care and control of blood sugar levels should be provided as early as possible. This can be done by diabetic educators and social workers.
Blood-sugar control: blood sugar control plan should be developed with the help of a primary care physician, podiatrist, and vascular specialist and should be based on the patient’s individual characteristics and disease severity.
Decreasing pressure: preventing further or new trauma by easing pressure to the area, which can be done with crutches, wheelchairs, and casting.
Peripheral vascular circulation improvement: drug therapy includes using antiplatelet agents. However, surgical intervention may be required.
Infection control or prevention: systemic and local control can be achieved using antibiotics and surgical wound cleaning.
Topical ulcer care: shallow ulcers can be managed with occlusive and semi-occlusive dressings that come in different forms and protect wounds from infection. In case of full-thickness ulcers, specialized dressing with hyaluronic acid and collagen is used, as well as surgical intervention for wound disinfection.
More details:
Prediabetes and measures of prophylaxis
Differences between type 1 and type 2 diabetes
Causes, mechanisms of the disease development and symptoms (Diabetes mellitus type 1)
Causes, mechanisms of the disease development and symptoms (Diabetes mellitus type 2)















Leave a Reply
You must be logged in to post a comment.