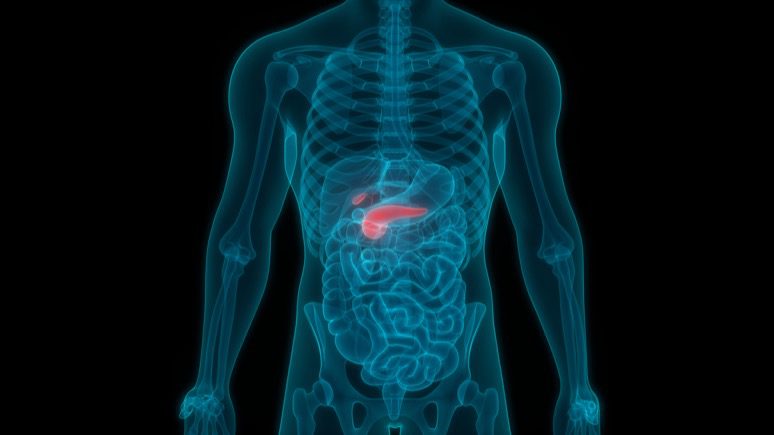
Inflammation of the pancreas is called pancreatitis. The pancreas is a flat, long gland. This gland is located next to your small intestine and behind the stomach in the upper abdomen. The pancreas produces enzymes helping digestion and hormones (insulin and glucagon) helping regulate how your body processes sugar (glucose).
Pancreatitis can be acute or chronic. Acute pancreatitis develops suddenly and lasts for a short time. In the case of chronic pancreatitis, the inflammation of the gland develops over many years. Usually, chronic pancreatitis occurs after an episode of acute pancreatitis. Treatment improves mild cases of pancreatitis, but severe cases can result in life-threatening complications.
Pancreatitis symptoms
You can experience different pancreatitis symptoms and signs, depending on your type of pancreatitis.
Acute pancreatitis symptoms
- Abdominal pain that spreads to your back
- Upper abdominal pain
- Rapid pulse
- Feeling of tenderness when touching the abdomen
- Fever
- Nausea
- Vomiting
Chronic pancreatitis symptoms
- Upper abdominal pain
- Weight loss without trying
- Abdominal pain that gets worse after eating
- Steatorrhea (oily, smelly stool)
Pancreatitis causes
Inflammation of the pancreas develops when digestive enzymes activate while still in the pancreas, irritating pancreas cells and causing inflammation.
Also, certain health conditions can cause pancreatitis. Such conditions include:
- Pancreatic cancer
- Specific medications
- Autoimmune disease
- Alcoholism
- Metabolic disorders
- Hypertriglyceridemia (high levels of triglyceride in the blood)
- Hypercalcemia (high blood calcium levels). Hypercalcemia can result from overactivity of the parathyroid gland (hyperparathyroidism)
- Gallstones
- Cystic fibrosis
- Injury to the abdomen
- Abdominal surgery
- Infection
- Trauma
- Obesity
Pancreatitis can also result from the treatment of gallstones by Endoscopic retrograde cholangiopancreatography (ERCP). A family history of pancreas disorders also increases your risk of pancreatitis development.
In some cases, pancreatitis cause cannot be determined. Such a condition is called idiopathic pancreatitis.
Acute pancreatitis treatment
In the case of an acute pancreatitis attack, you may receive strong pain relievers. Also, the doctor may prescribe you stomach drainage with a tube placed through your nose. A prolonged pancreatitis attack may require intravenous feeding and hydration.
You will likely need to stay in the hospital, where your physician can watch for you and provide treatment that includes:
- Antibiotic medications in the case of the infected pancreas;
- Pain medications;
- Intravenous (IV) fluids, given through a needle;
- Fasting or low-fat diet. In order for your pancreas to recover, you might need to stop eating (you will receive nutrition through a feeding tube).
In more severe cases of acute pancreatitis, the treatment might include:
- Endoscopic retrograde cholangiopancreatography (ERCP). In this procedure, a tube is inserted into the stomach and upper intestine to remove gallstones if they are blocking your bile or pancreatic ducts. The doctor makes a small cut in the bile duct to remove stones or insert a plastic tube (stent) into the duct to relieve the obstruction.
- Gallbladder surgery if your pancreatitis is caused by gallstones.
- Pancreas surgery to remove fluid or dead or diseased tissue.
Chronic pancreatitis treatment
If you have chronic pancreatitis, your physician will pay attention to managing pain and watching for complications that affect digestion. The doctor may prescribe you a pancreatic enzyme replacement therapy to restore the ability of the digestive tract to digest nutrients. Pancreatic enzyme replacement therapy may also decrease the frequency of new pancreatitis attacks.
For chronic pancreatitis treatment, you might need:
- Insulin for diabetes treatment
- Pain medications
- Pancreatic enzymes to help your body absorb enough nutrients from your food
- Surgery or procedure to relieve pain, help with drainage, or treat blockages
Anesthetic medications can be injected into the nerves near the spine to relieve pain. If the pain does not relieve in response to medication or nerve blocks, the doctor may surgically remove the damaged pancreatic tissue. However, such an option must be considered as the last report.
You can also use a Khavinson peptide supplement Suprefort to restore the proper functioning of the pancreas. Suprefort is a cytomax that contains peptide bioregulators of the pancreas. These peptide bioregulators affect pancreatic gland cells exclusively and do not affect other organs. Suprefort can restore the optimal functionality of the pancreas, normalize metabolism and the digestive system’s work.
Click here to read more about Suprefort.















Leave a Reply
You must be logged in to post a comment.