The diagnosis of multiple sclerosis disease is based on the presence of:
- at least two different lesions (plaques or scars) in the white matter of the CNS (the space dissemination criterion);
- at least two different episodes in the disease course (the time dissemination criterion);
- chronic inflammation of the CNS, as determined by analysis of the CSF (the inflammatory criterion).
There is also McDonald Criteria, which comprise five distinct possible presentations, as well as the additional information needed to illustrate the hallmark characteristic of multiple sclerosis, dissemination in time (DIT) and/or dissemination in space (DIS):
- two or more attacks (events typical of an acute demyelinating event in the CNS lasting at least 24 hours) with objective clinical evidence of two or more lesions or objective clinical evidence of one lesion with reasonable historical evidence of a prior attack;
- two or more attacks with objective clinical evidence of one lesion plus evidence of DIS: one or more T2-weighted lesions in at least two regions of the CNS typically affected by MS or another clinical attack implicating a different site;
- one attack with objective clinical evidence of two or more lesions plus evidence of DIT: simultaneous presence of asymptomatic gadolinium (Gd)-enhancing and non-enhancing lesion at any time; new T2-weighted and/or Gd-enhancing lesion(s) on follow-up MRI, irrespective of its timing with reference to a baseline scan; a second clinical attack;
- one attack with objective clinical evidence of one lesion (clinically isolated syndrome) and evidence of DIS and DIT as previously described;
- insidious neurologic progression suggestive of PPMS;
- one year of multiple sclerosis disease progression plus two of the following:
- evidence of DIS in the brain based on one or more T2-weighted lesion(s) in MS-characteristic regions;
- evidence of DIS in the spinal cord based on two or more T2-weighted lesions in the cord;
- positive CSF findings (isoelectric focusing evidence of oligoclonal bands and/or elevated IgG index).
The goal of the McDonald Criteria is to enable early diagnosis and prompt treatment. The criteria also simplify the demonstration of DIT and DIS with fewer MRI evaluations. In addition, the panel aimed to make multiple sclerosis easier to distinguish from the commonly misdiagnosed differential of neuromyelitis optica (NMO) and its spectrum disorders. The new criteria also improve the specificity and sensitivity of the original criteria and make the diagnosis more uniform to allow for widespread use.
The diagnosis procedure:
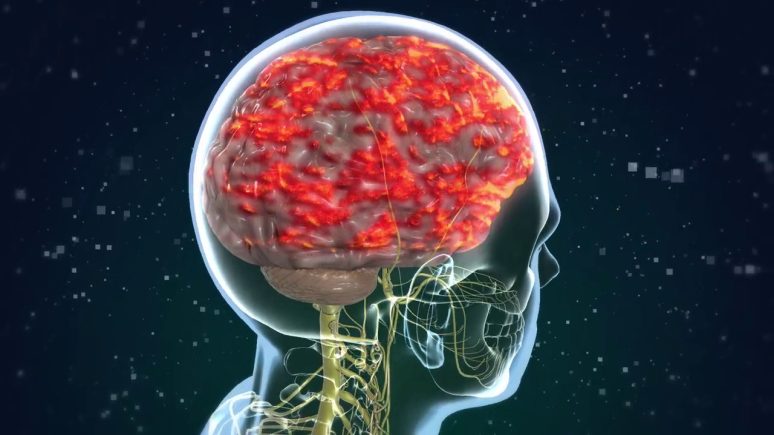
- checking for signs of damage in at least two separate areas of the CNS (the brain, spinal cord, and optic nerves);
- proving that the damaged regions appeared at least 1 month apart;
- eliminating other possible diagnoses;
- establishing the duration of symptoms for more than 24 hours, appearing as distinct episodes at least 1 month apart;
- performing an MRI;
- performing a spinal tap and examining for oligoclonal bands.
At autopsy, multiple, discrete pink or gray areas that have a hard, rubbery texture are discovered within the white matter. The lesions are natural occurrences that consist of myelin and oligodendrocyte loss areas, infiltrates of inflammatory cells, including lymphocytes and macrophages. The condition of axons and neurons within these lesions distinguishes MS from other destructive pathological processes that are accompanied by focal inflammation.
There are many signs of multiple sclerosis, including moderate-to-severe spasticity, mostly in the legs, that happens in more than 30% of patients, and unilateral numbness affecting one leg that spreads to affect the other leg, pelvis, abdomen, or thorax. Another common sign of MS is optic neuritis, meaning complete or partial loss of vision.
Sensory disturbances in multiple sclerosis patients:
- paresthesias (numbness and tingling);
- dysesthesias (burning and “pins and needles”);
- diplopia;
- ataxia;
- vertigo;
- bladder disturbances in more than 90% of patients;
- constipation in 30% of patients;
- sexual dysfunction;
- fatigue.
Sensory disturbances usually resolve, but sometimes evolve into chronic neuropathic pain, trigeminal neuralgia can also occur.
Click here to read more about treatment of the nervous system.















Leave a Reply
You must be logged in to post a comment.